Dementia Post #4 - Caring For the Caregiver, Coping Strategies
Cobra Chickens (aka Canada Geese) Echo Dale Boating Lake Aug 6 2025
I have not been a direct caregiver to someone with dementia but I have had a similar experience sort of in reverse caring for my late husband Carl when he had PICS (Post ICU Syndrome). I was also a caregiver to Carl when he had terminal cancer. I’m sharing some coping methods that helped me - I’m hoping that sharing my story might help others.
A list of resources is at the bottom of the article.
Being a Caregiver for a Person With Dementia Takes a Toll
I was lucky with Carl and his PICS (Post ICU Syndrome) - I knew the disturbing symptoms would get better. I have not experienced being a live-in caregiver for someone with dementia which comes with many more challenges. I’m lucky enough that when I go visit my dad (Dementia Dad), I can choose the time of day. Many people with dementia can get worse as the day goes on which can be extremely frustrating for the live-in Caregiver.
Maybe the person with dementia
has forgotten who the Caregiver is
forgets to turn off the taps or the stove
thinks the Caregiver is a threat and reacts violently
wanders at night; they might even leave the residence
This can take a massive toll on the Caregiver.
Mental Health Help Is Vital
One of the most important things you can do to care for yourself is to take care of your Mental Health. My experience was easy compared to what Caregivers of people with dementia go through. Without getting help with my mental health, things would have been much worse.
People think nothing of going to the doctor for a physical when there’s nothing wrong, we need to normalize seeing a mental health professional the same way. When your mind is not calm it affects your body, often slowing the healing process. It can also affect those around you.
Both Carl and I saw a BHC (Behavioural Health Consultant). BHCs are not psychologists or psychiatrists, they cannot prescribe meds but work with your doctor who can. You need a referral from a medical professional and they are typically attached to a clinic and/or a doctor. Visits are covered under Alberta Health Care and there is no limit on the number of visits. They can do in person visits or over the phone (I’m not sure if they do video visits.) Carl had been seeing ours since 2016, I started seeing her some months later. (Our BHC eventually saw most of our children which was great; she understood the family dynamic and could call us out on our BS.)
Carl was on life support for a month after being diagnosed with the flu in late 2016. (Long story short, he was in septic shock and not expected to live. They had me say goodbye in the ER .) I saw my BHC once a week while Carl was on life support, sharing feelings that I could not burden my family with. I believed it was my job to keep a brave face, to be positive.
I wasn’t fooling anybody; our kids saw right through that. They had their own family chat on a messaging app which excluded me. Brats. Traitors. Ungrateful wretches. Seriously though, it was a very good and healthy thing for them to do.
As Carl recovered, the appointments were further apart. Without the help of our BHC, we would have been a real mess. I still see my BHC once a month. It’s like talking to a friend who is obligated to keep all of your secrets.
Know When to Not Only Say No, but to Say Hell NO!
Dealing with family members who were wanting news was challenging so instead of calling, I posted regular updates on social media for all to see. I was already a mess, the thought of actually speaking to multiple people was unthinkable. I was already having trouble holding it together.
One of Carl’s children who was living in BC wanted to be able to call the ICU to get info on Carl.
I said
Hell NO!
The ICU did not have time to talk to all of the worried family members (Carl had 9 children altogether, 5 were from his previous marriages); they wanted only one family contact. I was his next-of-kin, I was the only one to talk to the ICU.
The same family member came out to visit (their idea, they had not been asked to come). They needed a ride from Calgary (3 hours away) because the car rental company would not accept their visa debit card as a credit card. This person was over 40 yo; I was not going to make a 6 hour round trip because of their piss poor planning. I gave them the number for the shuttle. They also wanted to be able to use my car in town or for me to drive them around; I handed them a bus schedule. I didn’t say hell no to their face; I knew they were worried about their dad and I did not need to make things worse. However, I was not going to cater to their needs, I was struggling enough.
Gather Your Chosen Supports Around You
If you want to have someone with you at appointments, by all means include them! It is best to minimize how many people will be speaking with the medical team. Not all family members can be trusted so pick the one you trust the most. The person you trust the most might not be a family member at all. If that is the case, make sure you have a Personal Directive, otherwise your next of kin makes all the decisions.
Let the medical staff know if someone is stepping over the line, they can have the person removed.
Life With PICS
Carl had to learn to walk, talk and eat again. The brain fog was considerable and bothered him very much. The other symptoms were also disturbing to him; it took Carl weeks to be able to hold a coffee cup without his hands shaking. Having to use a walker for months was annoying for a man who was used to being able to swing his leg over his Harley and go. Hearing the roar of other motorcycles depressed him because he knew he could not do it.
Carl would get easily frustrated at not being able to do the things he had been able to do all his life. He had bursts of anger which was surprising for a man who did not let much get to him. This improved as his brain healed. (Unlike people living with dementia, Carl had hope - he could see that improvement was happening every day.)
Sometimes You Need To Step Back To be The Most Help, Find Tools That Work
It was my instinct to immediately go and help Carl when I saw him struggling but I had to force myself to step back and let him do it on his own. I told him I would help if he wanted me to but it was better for him to try to do it himself (again, Carl was getting better). Sometimes it was too much and he asked me for help.
Sometimes I had to remind Carl to do his physical therapy. Carl had a wheelchair for when his artificial leg was off. It was very easy for him to wheel around the house and avoid standing or walking. I knew he should take every opportunity to stand and walk, even if it was only for a second. Nagging someone is not my style. Carl knew I was looking out for his best interest but he didn't like being nagged either. I put up signs around the house reminding him to stand up. They said
STAND UP
(nag, nag, nag)
It was not an order, it was a reminder. Some days it just was not going to happen. The signs helped; I was not nagging him all the time and he did not feel berated. Sometimes he would call out from the kitchen - “Yes, I’m standing up!” It was all in good humour and meant to make me smile.
Respite Care is Vital - Caregivers Need Care Too, Accept The Help
When Carl was diagnosed with stage 4 cancer, I had already been diagnosed with Caregiver PTSD. I had stopped sleeping in the same bed as Carl for a long time after he was released from the ICU because I would wake multiple times in the night to see if he was still breathing.
I lied to him and told him that I was restless and did not want to disturb him, that’s why I slept on the couch. I did not want to burden him with guilt, I knew it would make him feel bad and it certainly wouldn’t help me sleep any better. I didn't even tell my children until after he was gone in case they let it slip accidentally.
The demands on my energy were high. My kids hired a house cleaner to come in every week for me so I could spend more of my energy taking care of Carl. When my son and daughter in law came to visit from out of town, I used that opportunity to get away for a few days; they kindly offered to provide respite care. (Carl could fend for himself, I was just worried about the meds and his vitals.)
I was only to be contacted in case of an emergency.
(I was lucky - I had family to help me so Carl was not being left with strangers. Carl wanted me to go and rest, there was no resentment on his part. I wasn’t burdened with a guilt trip like many caregivers are.)
I left specific instructions for Carl’s care such as -
Before giving the blood pressure meds, check the blood pressure. A reading under (these parameters) means hold the meds.
Check his O2 level with the pulse oximeter. Depending on the O2 readings they were to call the doctor or an ambulance. (This saved him a number of times - when his O2 dropped like a rock, we knew he had pneumonia even before the infection showed up in the bloodwork, he was able to get IV antibiotics right away.)
If Carl was out of breath or unusually fatigued, check his blood pressure, and O2. If blood pressure was low, they were to give him fluids. If the O2 was below a certain point, they were to call an ambulance.
I booked a room in Drumheller for 2 nights, planning a visit to the Royal Tyrell Museum. I was so tired that I nearly fell asleep on the 3 hour drive to my hotel. I got to my room and slept for a day; I slept most of the next day too. I never made it to the museum, I was too exhausted to do anything that ambitious. I did stop on the way home for a hike, but that was all the sightseeing I got to do.
Never Underestimate Your Own Knowledge, Keep Medical History and Test Results Handy
My way of dealing with difficult situations is to learn as much as I can. I started reading up on ICU care techniques; the next year I read about the type of cancer he had, the different treatments and chemotherapies, etc. Sometimes I shared them with his team. I learned so much that multiple doctors and nurses thought I had medical training; they treated me more as a colleague than as a patient’s wife. I am not a medical expert, I have no medical training whatsoever. I was however, an expert on Carl. I taught myself enough to know and understand the terminology they used (which came in useful when I translated it into layman’s terms for Carl ), the different readings on the screens and when to be concerned.
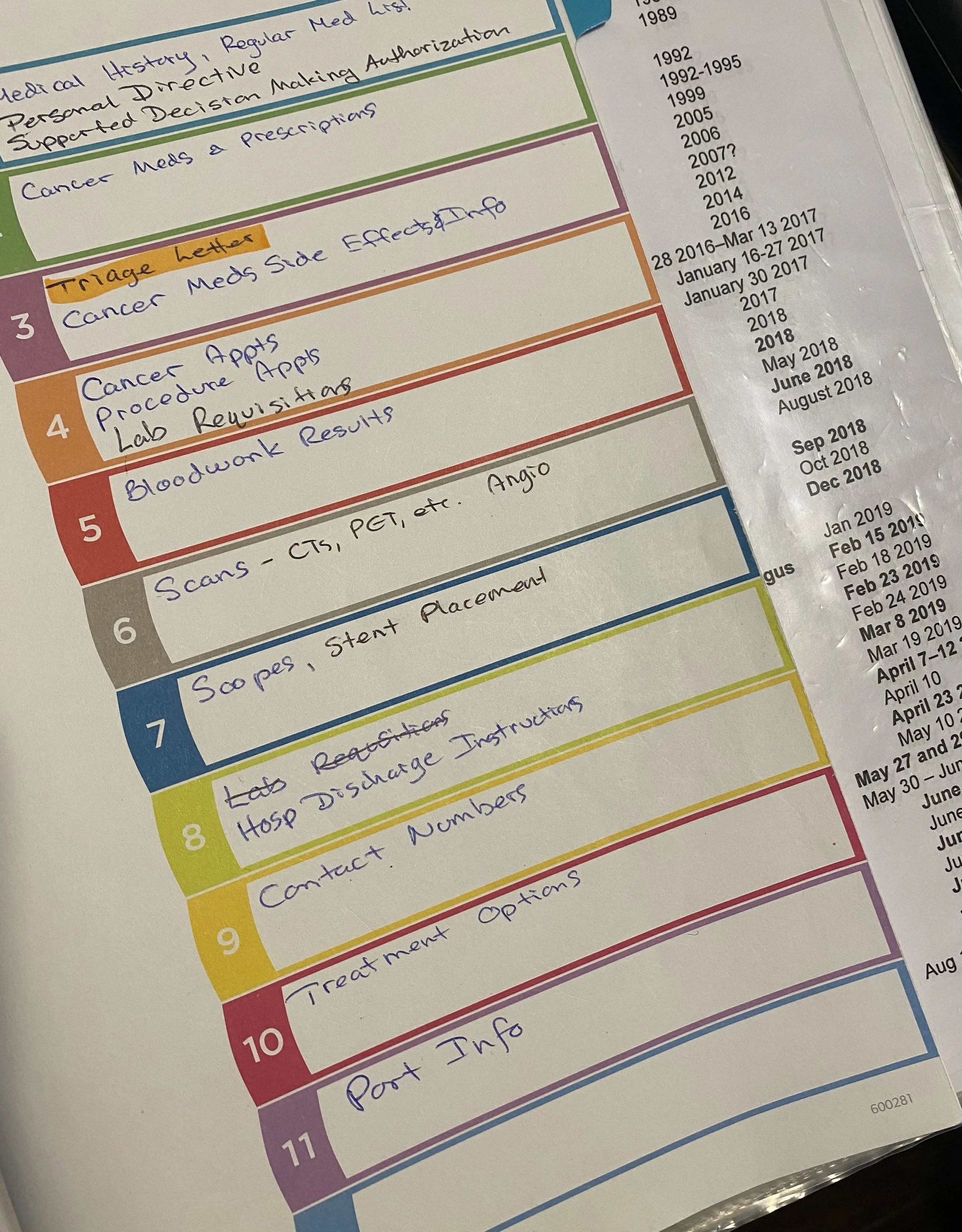
Photo of Carl’s Cancer Binder, I had one for his heart issues too. The page with the dates was his medical history.
I started collecting all his medical information and putting it in a binder using sheet protectors. The info stayed pristine and nothing fell out.
The things that were used the most were the medical history and the medication list. Carl’s medical history was extensive so I did two versions - one was chronological, the other was grouped by category.
Cancer
Cardiovascular and Respiratory
Endocrine and Genitourinary
Trauma Surgeries
Other Surgeries
Recent Infections and Admissions
Other Condition and Procedures
I had multiple copies made up to give to medical staff to keep, they very much appreciated it. It saved a lot of time and I did not have to try to remember anything during a crisis (and there was always a crisis).
Most people don’t have to get as detailed as I did. For most people, something much simpler will work; Carl’s medical history was extensive and complicated.
Here’s one example of how useful the binder was. On one trip to the ER, the doc started talking about a 12 inch (30cm) long tumour. I knew that was completely wrong. Because I had Carl’s cancer binder with me with all of his test results, I was able to show the doc that tumour was 12 inches down, not 12 inches long.
I probably could have accessed the information online (and sometimes I did) but it was simpler for me to have the binder handy. I also left it in Carl’s room whenever he was admitted so staff could use it too.
Cherish the good Times
The good times are sometimes few and far between, make the most of them. Sometimes it is the little things that count the most. It can be something as simple as enjoying a cup of coffee or a sunset or listening to music together.
This is a good memory, being under that enormous tree with Carl. It was incredibly peaceful.
Carl at St Joe’s in Medicine Hat, October 2019. This American Elm tree was 113 years old when this photo was taken. It is still alive, and still just as beautiful!
Resources
Medicine Hat Behavioural Health Consultants Where to find them
Local Resources Palliser PCN Lots of good resources here
Alzheimer Society - again, lots of good resources
Health Link Alberta -Scroll down for info about dementia
RAMP - Residential Access Modification Program - financial assistance with home modifications - it can be used to make your home safer
Alberta Aids to Daily Living - The Alberta Aids to Daily Living (AADL) program helps Albertans with long-term disabilities, chronic illness or terminal illness. The program provides funding for basic medical equipment and supplies so clients can live independently at home and within their communities.